Search for topics or resources
Enter your search below and hit enter or click the search icon.
October 29th, 2025 | 4 min. read

Many things in healthcare are up for debate, like whether coffee is a health elixir or a guilty pleasure, or if dairy deserves a place in the fridge.
But there’s one topic everyone agrees on: We need more access to primary care, and the data backs it up, says Dr. Nirav Vakharia, chief operating officer at Marathon Health.
“Number one, it’s the only health service proven to improve clinical outcomes for a population, lower hospitalizations, lower cost, and have a positive ROI,” Dr. Vakharia says. “Number two, it saves lives. For every 10,000 people to whom you add one primary care provider, that group lives two months longer and has a 1% lower risk of cardiovascular or cancer risk. And number three, the more you use it, the better things get for everyone.”
That was the driving message behind Dr. Vakharia’s keynote—Sparking excellence: Our care model—delivered during the company’s annual ENGAGE 2025 event.
Dr. Vakharia says no one’s arguing whether better access to quality primary care improves lives. Yet, for far too many people, it’s still out of reach, and the problem is only getting worse.
“When you do get in to see a provider, you spend 11 minutes, because their job is completely unsustainable,” he says. “We have the accumulation of so much deferred and delayed care from the pandemic that we're seeing an epidemic of advanced cancer diagnoses. Things that should have been earlier-stage cardiovascular risk are now showing up as heart attacks and strokes.”
Delaying primary care creates a domino effect of problems, from more bankruptcies and rising chronic disease to longer wait times, eroding trust, and higher suicide and maternal mortality rates.
Over the past few decades, Dr. Vakharia says patients have slipped down the priority list in the healthcare system. They’ve been overshadowed by insurance companies, health systems, big pharma, device manufacturers, and even the government.
“We have an opportunity to move them to the front of the line and listen to the heart of the matter,” he says. “Envision taking all that negative energy and refocusing it on what really matters.”
Dr. Vakharia says the healthcare industry can take a lesson from Starbucks.
“They have 40,000 stores around the world. Thirty million people walk into a Starbucks every day and they pick from 170,000 potential drink combinations. And yet, you walk out with what you want. How do they do that?"
“I'm not trying to compare healthcare to making a grande caramel macchiato with no foam, an extra pump of caramel, half almond, half soy in a venti cup,” he adds. “But there are things we can learn around how we bring mass customization so that the individual gets what they need.”
The iron triangle of healthcare
Dr. Vakharia likens Marathon Health’s approach to building a primary care model to crafting a recipe, because a recipe leads to a predictable outcome.
It starts by choosing the right ingredients, such as clinical programs and services that reflect the unique needs of each population and are designed to drive measurable results.
In primary care, he says a well-balanced recipe leads to a concept known as the “iron triangle” of healthcare, creating a balance of accessibility, quality, and affordability.
Dr. Vakharia says two major misconceptions have long surrounded the iron triangle of healthcare. The first claims that improving one element automatically harms the others. The second insists that you can only achieve two sides of the triangle, but never all three.
“That’s been the dogma for 40 years,” he says. “I'm going to make a bold proposition that in our partnership, we can actually have all three, because we'll rewrite that recipe for our care model. We're going to break three myths that have governed this for decades.”
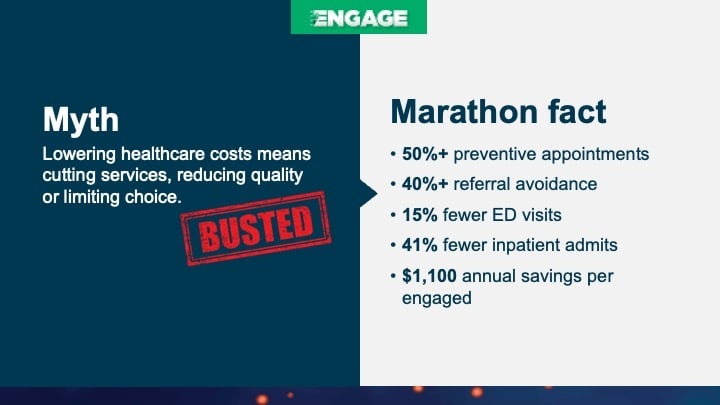
Myth #1: Lowering healthcare costs means cutting services, reducing quality, or limiting choice
Dr. Vakharia says many employers believe the only way to control costs is by cutting services. At the same time, employees often get pushed toward pricey surgeries when lower-cost options, like physical therapy, could deliver the same results.
“We've got to invest in the right services in order to save money in the long-run,” he says. “By having advanced primary care that's more focused on prevention than reaction, you're helping to lower your ER, inpatient, and specialty utilization, which drives savings.”
In fact, Marathon Health data shows customers who implement an advanced primary care program see tangible results, including roughly $1,800 annual savings per employee, 42% reduction in ER utilization, a 40% in referral avoidance, and a significant uptick in preventive visits.
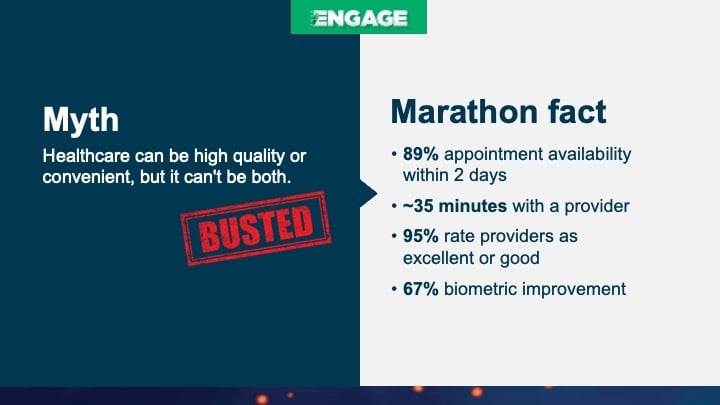
Myth #2: Healthcare can be high quality, or it can be convenient, but it can't be both
Dr. Vakharia says employers need to push back on the idea that accessible, convenient primary care is somehow low quality. In reality, the right care model can deliver both, making it easy to access while maintaining exceptional standards and outcomes.
“We have great accessibility. When you come in, instead of spending 11 minutes, we're spending on average 35 minutes. What do we do with all that extra time? We expand the scope of services. We help people stay out of the specialist office, stay out of the emergency room.”
“I certainly wouldn't want a mechanic to spend 11 minutes diagnosing and fixing my car and driving off. I don't know why we tolerate that for ourselves either,” he adds.
With Marathon Health, patients spend more time with their providers and can usually schedule same- or next-day appointments, making it easier to get the care they need when they need it. By combining onsite, nearsite, and virtual options, Marathon Health improves access, outcomes, and overall employee satisfaction.
“In terms of increased quality, we're all on one electronic health record now and we have the ability to monitor our prescribing patterns, our lab ordering patterns, what kind of imaging we’re ordering, and what referrals we’re making to the community,” he says. “We make sure we're more within the guidelines, more evidence-based.”
While we may applaud the personalization of a Starbucks order, Marathon Health’s care model actually enables employers to tailor services to best meet the needs of their workforce. Providers are encouraged to form trusted, meaningful relationships with employees, get buy-in, and design personalized care plans that inspire employees to take charge.
“Here's one thing I've learned about driving change: People love to change when it's their choice,” Dr. Vakharia says. “People don't like to be changed.”
Through Marathon Health’s personalized care model, employers on average see over 70% employee engagement—including more than 50% for high-risk employees—while earning a 90+ Net Promoter Score.
“We can't run the risk of feeding the myth that personalized healthcare is not possible,” he says. “That’s what I call our red line—personalizing to your patient population, personalizing to the individual patient. We want to continue to make sure that stays central to our care model.”

If Dr. Vakharia’s insights inspired you this year, just wait until ENGAGE 2026. He’ll return with a brand-new session, Tectonic shifts in healthcare: Emerging treatments, tech, and trends, exploring how innovation is transforming care delivery and redefining the healthcare experience.
ENGAGE 2026 kicks off February 25th in Colorado Springs. We can’t wait to engage again!